Survival and importance of early action
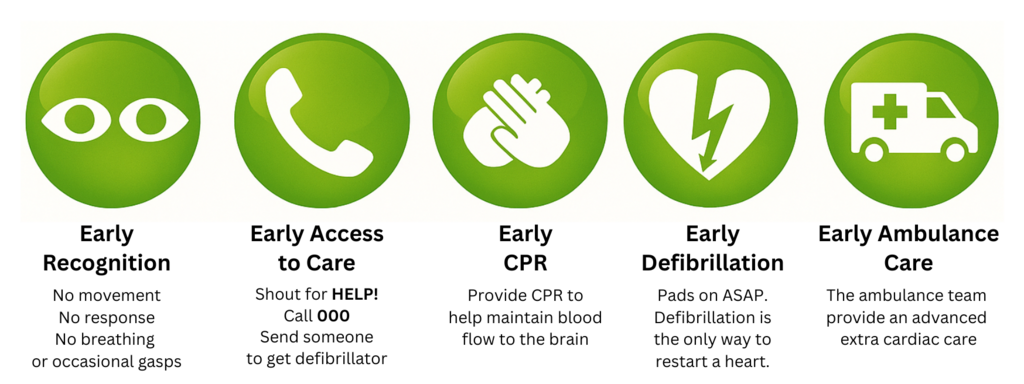
In Australia, survival from VF cardiac arrest depends on immediate action:
- Recognise Cardiac Arrest - No movement, No response, No breathing or occasional gasps.
- Get help - Sout for HELP!, Call 000, Send someone to get a defibrillator.
- Start and maintain CPR - Provide CPR to help maintain blood flow to the brain.
- Defibrillate as soon as possible - Pads on ASAP. Defibrillation is the only way to restart a heart.
- Early Ambulance Care - The ambulance team provide an advanced extra cardiac care.
Every minute without defibrillation reduces survival by about 7–10%. Early bystander CPR and AED use are the strongest predictors of survival with good neurological recovery.